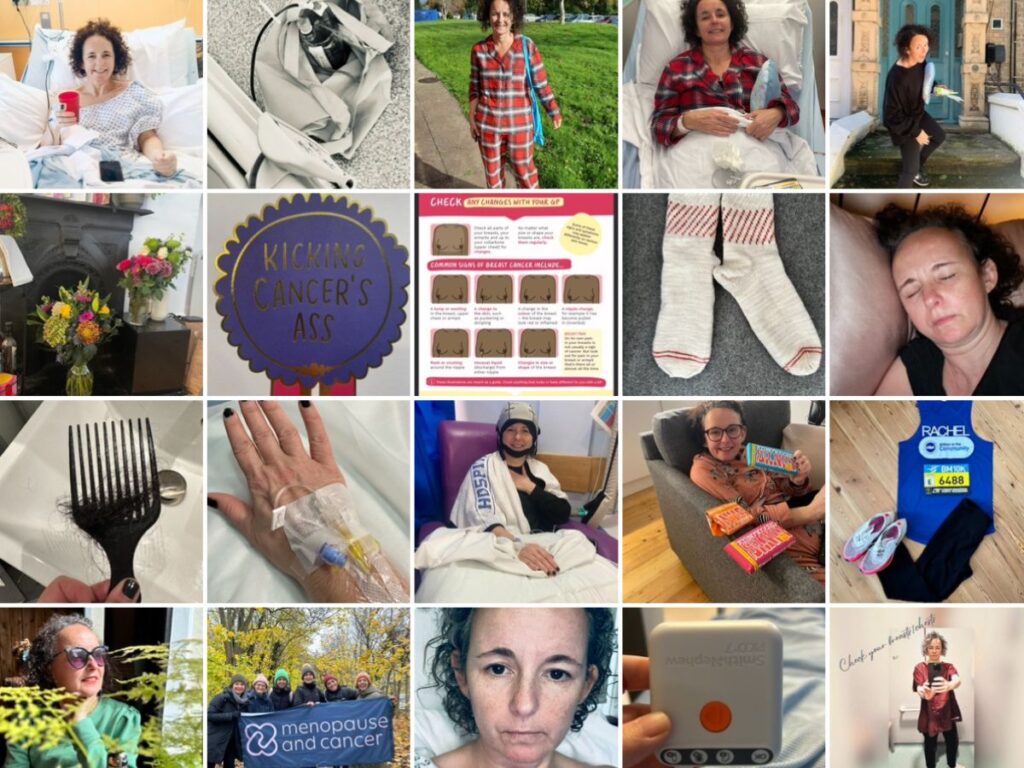
When I was first diagnosed with breast cancer in September 2022, I underestimated just how much I would learn in the coming months, years about breast cancer, treatment and well-being in general.
Note: the below is based on my own experience, its not medical advice, just the things I’ve learned which may be useful to know…
01
It’s not just Breast Cancer there are so many types
I heard recently there are 48 different types. Before diagnosis, I was vaguely aware of something called Herceptin (I now know this is a drug to treat Her-2 positive breast cancer). I knew hormones may have a part to play and that HRT had an unfairly bad rep where breast cancer was concerned. I did not realise there were so many types. Firstly there are the positives and negatives – whether hormones or a protein called HER2 is involved in the growth of breast cancer cells – there can be a mix, and in some instances none (you’ll hear this termed as Triple Negative). And then there is where it’s growing in the breast.
After I was diagnosed with grade 2 invasive ductal carcinoma (Hormone receptor positive and HER2 negative), one of the most common types of breast cancer, I fervently googled those string of words written on the letter explaining my biopsy results. I came across plenty of other types: invasive lobular cancer, ductal carcinoma in situ, lobular carcinoma in situ, inflammatory, pagets disease – to name a few. It was confusing but Breast Cancer Now explains it all clearly here.
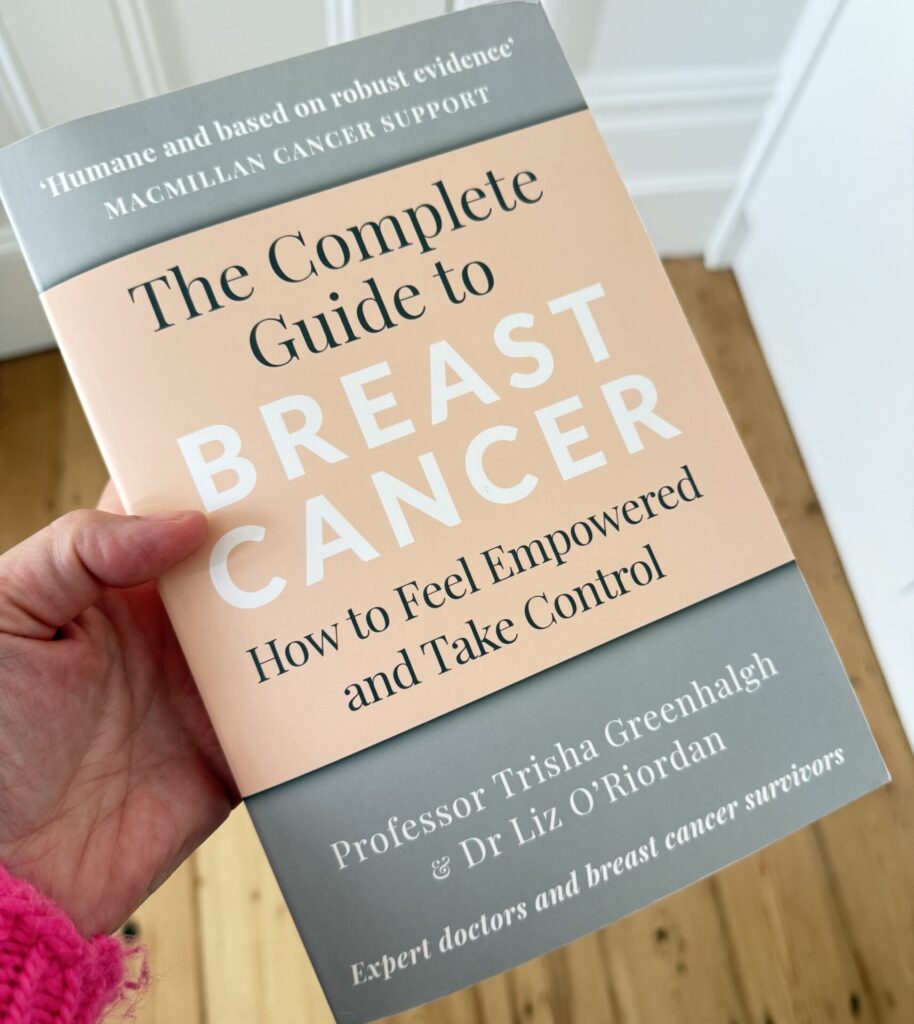
And I also invested in this gem of a book – The Complete Guide to Breast Cancer
02
I found myself asking are grades and stages the same thing?
In short no grade and stage are not the same. I had never heard the term ‘grade’ before and it’s easy to misunderstand if you’re not in the know. A family member helpfully told their friends that I had stage 2 cancer after reading one of my many medical letters when in actual fact it was grade 2. To summarise, a grade is how fast the cancer cells are multiplying (there are 3), whereas a stage is how far it may or may not have spread beyond the breast.
03
A mammogram alone cannot definitively tell if you have breast cancer, but its super good for early detection.
Its just one of many procedures you’ll have. I found a lump, I hadn’t reached the age of a routine mammogram. I was assessed by a GP who referred me to a breast care centre where I was then assessed by a specialist nurse. I had a mammogram, then more mammograms before having an ultrasound and biopsy – which were enough to diagnose me. A few weeks later I had a stereo core biopsy (probably the most painful of all the tests and not something everyone has to endure, thankfully).
04
Its not a one size fits all for breast cancer treatment, and it also can change along the way.
I was told at the outset, you will need surgery and endocrine treatment. My treatment plan in reality was different.
The first thing I had, was surgery – a mastectomy. A breast care nurse or someone in your healthcare team will take you through your options. This can be quite hard and overwhelming because you need to make decisions and think about how you feel as well as being clear about what is right for you. I was very sure I wanted to have a breast and not be flat, if that was an option. My decision here was whether to have a reconstruction using my stomach tissue (there’s not a lot of it!) or with an implant. I opted for the reconstruction with stomach tissue only to discover I didn’t have enough blood vessels to make it viable. Implant it was. (Curve ball number 1).
And then when I received the histology results – and good news, the cancer was gone – I was offered an Oncotype DX test to assess my risk of recurrence. (Curve ball number 2). And that came back with a medium to high risk of recurrence and the safest option, was to have chemotherapy (Curve ball number 3). The curve balls continued on into my second dalliance with breast cancer.
What I am saying here is even when you think you have a plan, it can change so if you can, take everything as it comes – one step at a time.
05
Genetic testing & Genomic Testing
Depending on your family history or the type of cancer you have, you may be offered genetic testing to assess if you have an increased breast cancer risk due to a faulty gene.
And if you have a specific type, stage and grade of cancer you may be offered an Oncotype DX test.
It’s unlikely there is a faulty gene given my history and type of cancer but I was eligible for an Oncotype DX test. This is a test which looks at the genomic make up of a tumour and assesses the risk of recurrence.
I am ever so grateful these tests are available.
06
Be prepared with your questions
This is easier said than done. I have often gone to an appointment expecting to be told certain information only to be blindsided by something new and unexpected. I would recommend preparing a list of questions for what you hope will be discussed. Invite someone to come with you to any appointment too – it’s particularly helpful so that if you are blindsided by the information shared by your healthcare team then you have someone to take notes and help you understand. You can always follow up, you can always ask for another appointment and you always have the right to a second opinion.
In my case, I was allocated a breast care nurse, who I could phone for further information. But also Breast Cancer Now have a telephone line with nurses on hand to offer support and at times I found this support more helpful.
07
You can have a recurrence in the same breast after a mastectomy
Although the majority of breast tissue is removed, there may be residual breast tissue and microscopic breast cancer cells can still be present. Less than a year after my mastectomy and a few months after finishing chemotherapy and whilst on endocrine treatment, I noticed a lump in the edge of my mastectomy scar. I assumed it was scar tissue. I stumbled across an instagram post which talked about signs of a local recurrence and that’s when I realised I should get this new lump checked. I went through the process again but I skipped straight to a breast ultrasound and fine needle aspiration because you can’t have a mammogram after a mastectomy.
Its unusual for this to happen after a mastectomy, I’m now more aware and continue to check monthly for any changes.
08
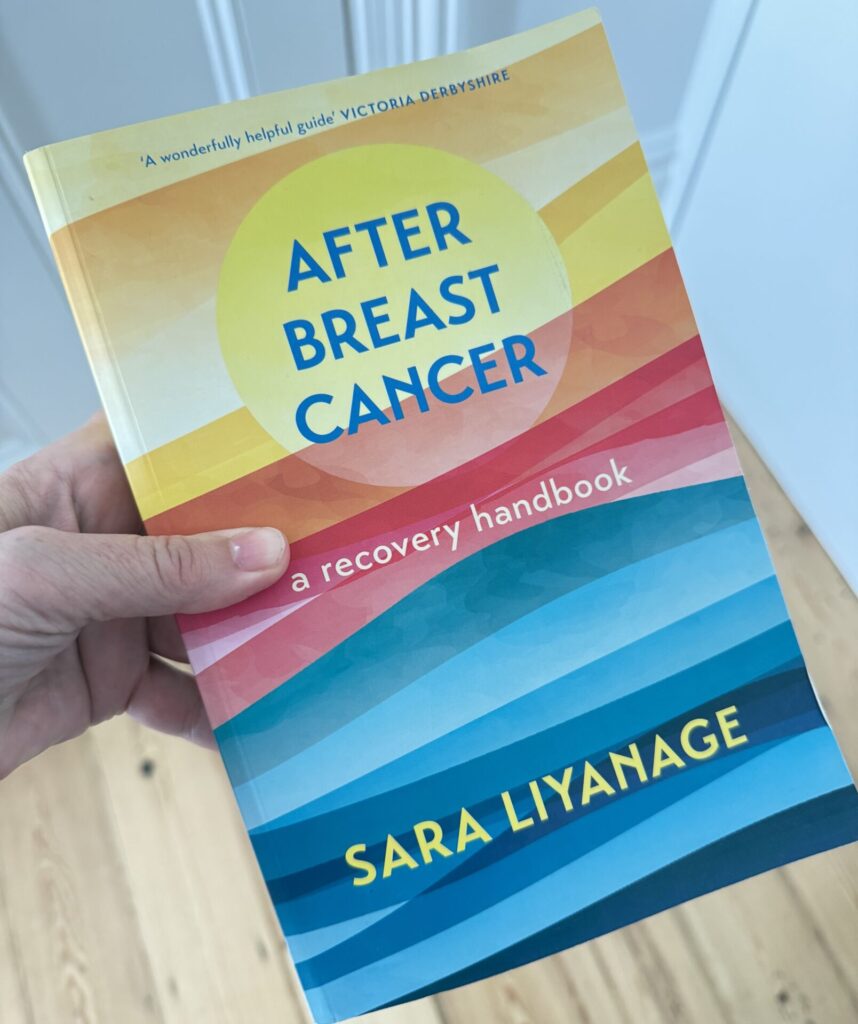
Recovery takes a long time after treatment has ended, and it’s not just physically.
I thought after my chemotherapy had ended I would feel back to normal a few weeks later. I was wrong. I was so up and down in terms of energy levels and fatigue (not to mention grappling with the near constant menopausal symptoms). I really tried to push through a lot of this, which on reflection was probably not the best idea. As well as physical symptoms, there were also emotional and psychological side effects, particularly an increase in feelings of anxiety and a decline in confidence. Not the best when you’re trying to work and get to some sort of normal.
And I learned radiotherapy, whilst a less invasive treatment compared to my chemotherapy, also had lasting side effects of fatigue. Although, this time round and as part of my second lot of treatment and a year after chemo, I was much better at resting when I needed.
Its important to continue to be kind to yourself and listen to what your body needs. I’m still learning this one, if I’m being truthful.
09
Treatment may push you into menopause
Chemotherapy can trigger a temporary menopause, or even push you permanently into it. Most people with ovaries are offered Zoladex, a monthly injection that temporarily stops the ovaries from producing estrogen and helps protect them during chemotherapy. For some women, these injections continue as part of ongoing endocrine treatment.
For me, the hot flushes started almost instantly after my first Zoladex injection, alongside a whole host of other symptoms I wasn’t warned about.
Breast cancer patients with hormone receptor-positive cancer are often prescribed medication like tamoxifen or an aromatase inhibitor to reduce the risk of recurrence (endocrine treatment). These medications can cause menopause or bring on menopausal symptoms. These side effects can be quite challenging to manage, and the treatments are usually prescribed for many years.
There is often little warning or guidance for people who experience menopause as a result of their cancer treatment. A fantastic organisation called Menopause and Cancer, which I’m proud to be part of, and works to support people in this area.
If you experience debilitating side effects from medication, speak to your healthcare team. There’s often an alternative treatment available.
10
A few other things I learned
I suddenly knew alot of things about breasts and found myself saying the word ‘breast’ ALOT!
It’s a tough thing to navigate — for everyone — and even those who’ve been through it can find it hard to get the words right. When you’re first diagnosed, it can be hard for others to know what to say. Sometimes, well-meaning words or advice don’t quite land as intended. I’ve learned that most people just want to help, even if it comes out a little clumsily.
I ended up with a whole new network of friends and support. I joined various groups and looked for organisations who I could turn to. This has been one of the best things about my experience. I’ve found these groups and communities to be a source of positivity – there’s something about being able to speak openly to people who have also had a similar experience. And I’ve made new friends.
You need to use your cancer card – it can open up some well deserved and at times much needed perks!
Dark humour can emerge.
Some of the medical terms will annoy you – I had rage at my recurrence being called superficial, there’s nothing superficial about cancer! But that’s medics for you!!
No one talks about the drain – after my mastectomy, I woke up with a drain hanging off me. I’m squeamish and this was not pleasant at all. It did mean I was very up tight because of it, and probably one of the reasons I ended up with a frozen shoulder. So another tip – do your exercises!
Fear of recurrence will live with you forever (but I hope it will fade) – I don’t know anyone who has had breast cancer who hasn’t then worried about a headache, a sore knee or had to get another lump checked. I recently had a lump in my armpit, it took me a few weeks to garner the energy, a bit scared about whether I could go through it all again, but I got it checked and it was just fat. Phew.